Dialectical Behaviour Therapy (DBT) is a powerful treatment approach that has gained recognition for its effectiveness in addressing a wide range of mental health challenges.
Developed by Dr. Marsha Linehan in the late 1980s, DBT was initially created to treat individuals with Borderline Personality Disorder (BPD). However, its success in treating BPD paved the way for its application in other mental health disorders as well.
In this blog, I’ll explore some of the applications of DBT, mainly focusing on my own direct experience with DBT as a treatment for Borderline Personality Disorder, but also touching on other conditions that this approach can support.
This is a personal dive into the options out there for people, and why I truly believe DBT can support and even completely transform life for at least a few of us out there. I can’t recommend a treatment plan for you, but I can give you my insight to a few mental health struggles and the application of DBT to them.
Let’s get started.
Understanding Dialectical Behaviour Therapy (DBT)
DBT is a therapeutic approach based on a cognitive-behavioural therapy (CBT) that also integrates ideas from Eastern philosophies and core principles of mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness.
DBT operates on the biosocial theory that if we have not been taught effective coping skills growing up, we can often struggle with regulating emotions and behaviours, leading to difficulties in managing interpersonal relationships and coping with distressing situations.
One of the distinguishing features of DBT is its emphasis on both acceptance and change. It encourages individuals to accept themselves and their current circumstances while simultaneously working towards behavioural change and emotional regulation. This dialectical approach forms the foundation of DBT and sets it apart from other therapeutic modalities.
Mental Illnesses Treated by DBT
Borderline Personality Disorder (BPD)
BPD is characterised by instability in mood, self-image, and interpersonal relationships. Individuals with BPD often experience intense emotions, impulsivity, and a fear of abandonment. DBT has been extensively researched and proven effective in treating BPD symptoms, helping individuals learn skills to manage their emotions, improve relationships, and reduce self-destructive behaviours.
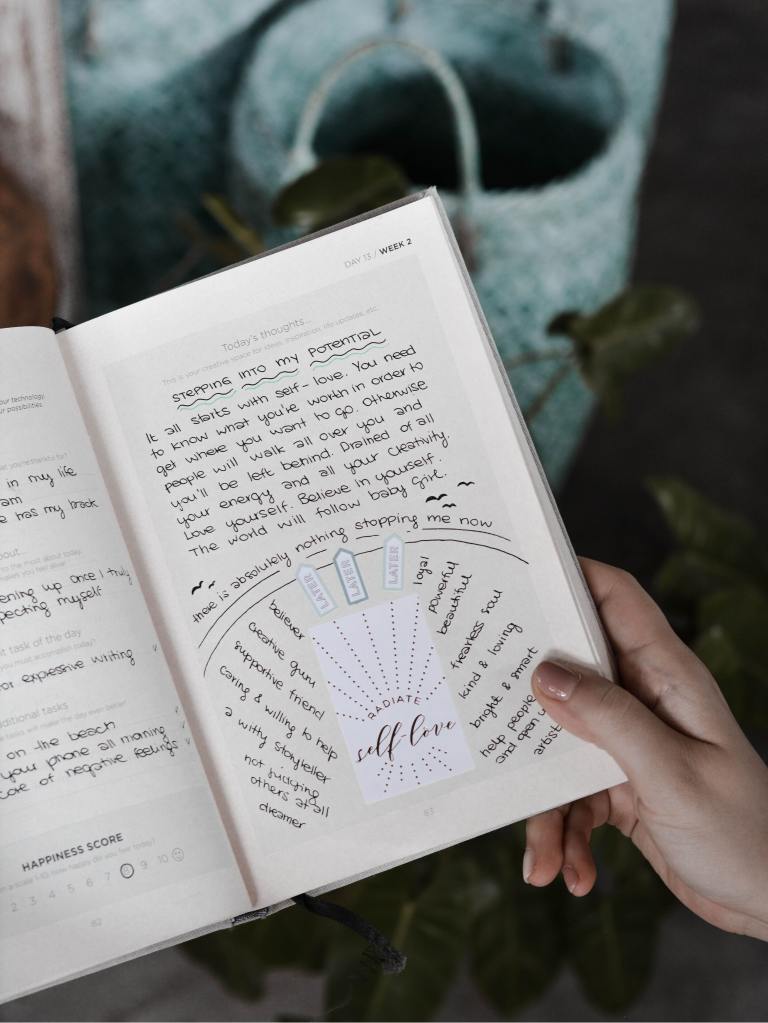
My own experience undergoing intensive DBT training as part of the treatment plan for my BPD highlights the transformative power of this therapy. Journaling also played a crucial role in my BPD recovery journey, providing a safe outlet to express my emotions and track my progress throughout treatment. BPD journal prompts, tailored to encourage self-reflection and emotional regulation, complemented the DBT skills I learned in therapy.
Complex Post-Traumatic Stress Disorder (C-PTSD)
While C-PTSD still isn’t recognised in the DSM-5 as a distinct condition, Complex Post-Traumatic Stress Disorder (C-PTSD) can develop after prolonged exposure to traumatic events, such as ongoing abuse, bullying, neglect, or captivity.
Unlike PTSD, which typically stems from a single traumatic incident, C-PTSD is characterised by a pattern of enduring traumatic events or surroundings, often occurring in childhood or over an extended period of time.
Individuals with C-PTSD may experience a range of symptoms, including emotional dysregulation, dissociation, difficulty trusting others, and disturbances in self-perception. These symptoms can significantly impair daily functioning and impact relationships, work, and overall quality of life.
In my own personal, non-medical opinion, C-PTSD is likely comorbid to many other mental health conditions or illnesses. For example, I think C-PTSD was underlying my presentation of BPD, and the C-PTSD is something I am still using DBT skills for on an ongoing basis, unlike with my BPD recovery, where I would be unlikely to meet the diagnostic criteria anymore.
That’s why I’ve dived into a bit more detail on the applications of DBT to C-PTSD specifically below. I really think that most people could find value in this.
Applications of DBT for C-PTSD
Dialectical Behaviour Therapy (DBT) offers a comprehensive approach to addressing the complex symptoms of C-PTSD. By integrating elements of mindfulness, distress tolerance, emotion regulation, and interpersonal effectiveness, DBT provides individuals with practical tools to navigate the challenges associated with trauma recovery.
- DBT Mindfulness and Grounding Techniques: DBT emphasises mindfulness as a core skill for managing distressing emotions and reducing reactivity. Through mindfulness practices, individuals with C-PTSD can learn to cultivate present-moment awareness and develop greater tolerance for uncomfortable sensations and emotions. Grounding techniques, such as grounding exercises and sensory awareness, can help individuals stay connected to the present moment and alleviate symptoms of dissociation when it is no longer an effective coping method in our lives.
- DBT Emotional Regulation Skills: C-PTSD often involves intense emotional experiences, including feelings of shame, guilt, anger, and fear. DBT teaches individuals how to identify and regulate their emotions effectively, allowing them to navigate triggering situations with greater resilience and self-control. By learning strategies to manage emotional arousal and respond adaptively to stressors, individuals can break free from the cycle of emotional dysregulation common in C-PTSD.
- DBT Interpersonal Effectiveness Skills: Trauma can profoundly impact relationships, leading to difficulties in establishing boundaries, communicating needs, and trusting others. DBT helps individuals develop interpersonal effectiveness skills, such as assertiveness, active listening, and conflict resolution, to enhance their relationships and establish healthy boundaries. By improving interpersonal skills, individuals with C-PTSD can cultivate supportive connections and create environments conducive to healing and growth.
- DBT Distress Tolerance Skills: Additionally, DBT equips individuals with distress tolerance skills to cope with intense emotions and distressing situations without resorting to harmful behaviours. These skills include distraction techniques, self-soothing strategies, and crisis survival skills, providing individuals with alternative ways of coping with overwhelming emotions and triggers.

Substance Use Disorders (SUD)
SUDs often co-occur with other mental health disorders and can exacerbate symptoms if left untreated. DBT provides a comprehensive approach to addressing substance use issues by addressing underlying emotional dysregulation and teaching coping skills to prevent relapse. By focusing on building distress tolerance and enhancing interpersonal effectiveness, DBT helps individuals develop healthier ways of coping with stressors, reducing the risk of substance misuse.
Journaling in the context of SUD recovery serves as a tool for self-monitoring and relapse prevention. By documenting thoughts, cravings, and triggers, individuals can identify patterns of behaviour and develop strategies to overcome challenges on their recovery journey.
Read more: 1000 Days Alcohol-Free: What I’ve Learnt
Eating Disorders
Eating disorders, such as bulimia nervosa and binge eating disorder, are complex conditions that require a multifaceted treatment approach. DBT offers skills training to help individuals regulate eating behaviours, manage emotions related to food, and improve body image.
By combining elements of mindfulness and behavioural therapy, DBT can help us address the underlying psychological factors contributing to disordered eating patterns, as well as help us take small, mindful steps in the way that is right for us.
For example, when I was in DBT I was struggling with my eating. One ‘Opposite Action’ and ‘Building Mastery’ challenge my therapist set for me was to eat a tangerine at the same time every day early in the morning. I tracked emotions, raw thoughts, sensations, urges. But I kept at it, journaled my way through it, and worked through all of those complexities in my individual sessions.
I found journaling to be a huge help in exploring my relationship with food, identifying triggers for disordered behaviours, and documenting progress in recovery. By recording thoughts and emotions surrounding eating habits, we can gain insights into maladaptive patterns and work towards developing a healthier relationship with food and body image, and healthier patterns of behaviour alongside that.
Integration of Journaling in DBT & Mental Health Recovery

Journaling serves as a valuable adjunct to DBT for individuals living with mental illness or in recovery. They not only provide a safe means of processing traumatic experiences—with support from the right therapy practitioner—but also help with tracking progress in DBT, learning the skills and fostering a greater sense of self-reflection.
DBT-informed journal prompts can guide individuals in exploring their emotions, identifying triggers, and challenging maladaptive beliefs associated with trauma. By incorporating journaling into their daily routine, individuals can deepen their understanding of themselves and their recovery journey, promoting healing and resilience in the face of C-PTSD, BPD or other mental health conditions.
Final Thoughts
In conclusion, DBT is a versatile therapeutic approach that offers hope and healing to individuals struggling with various mental health challenges. Whether it’s BPD, PTSD, SUDs, or eating disorders, DBT provides effective tools and strategies to promote recovery and enhance overall well-being.
If you or someone you know is grappling with mental health issues, remember, you are not alone on your journey towards mental health and well-being. Reach out for support, and remember that recovery is possible. You can also consider exploring DBT as a treatment option and incorporating journaling as a supportive tool in the recovery process.
Throughout my year in therapy, I crafted a guide to the core skills that underlie all of DBT: DBT Mindfulness Skills. My guide is only a few pounds/dollars, and goes beyond the basic clinical point of view, offering you a personalised guide enriched by real-life examples from my own journey with DBT and the core skills.




2 thoughts on “What Mental Illness Does DBT Treat?”